Neuropathies explained
A deep dive into peripheral and cranial neuropathies and how I go about treating them
Discover how electro-acupuncture can support nerve repair and regulation in both peripheral and cranial neuropathies. I explores the science behind neuropathy, different types of nerve fibers, and how targeted electro-acupuncture treatments can help restore healthy nerve function—with a special focus on conditions involving the vagus nerve.
Neuropathies explained- A neuroscience lens
Neuropathies refer to a broad category of nervous system disorders that arise from damage or dysfunction of nerves outside the central nervous system, including both peripheral nerves and cranial nerves. These nerves serve as the body’s communication highways, transmitting signals between the brain, spinal cord, and every tissue and organ.
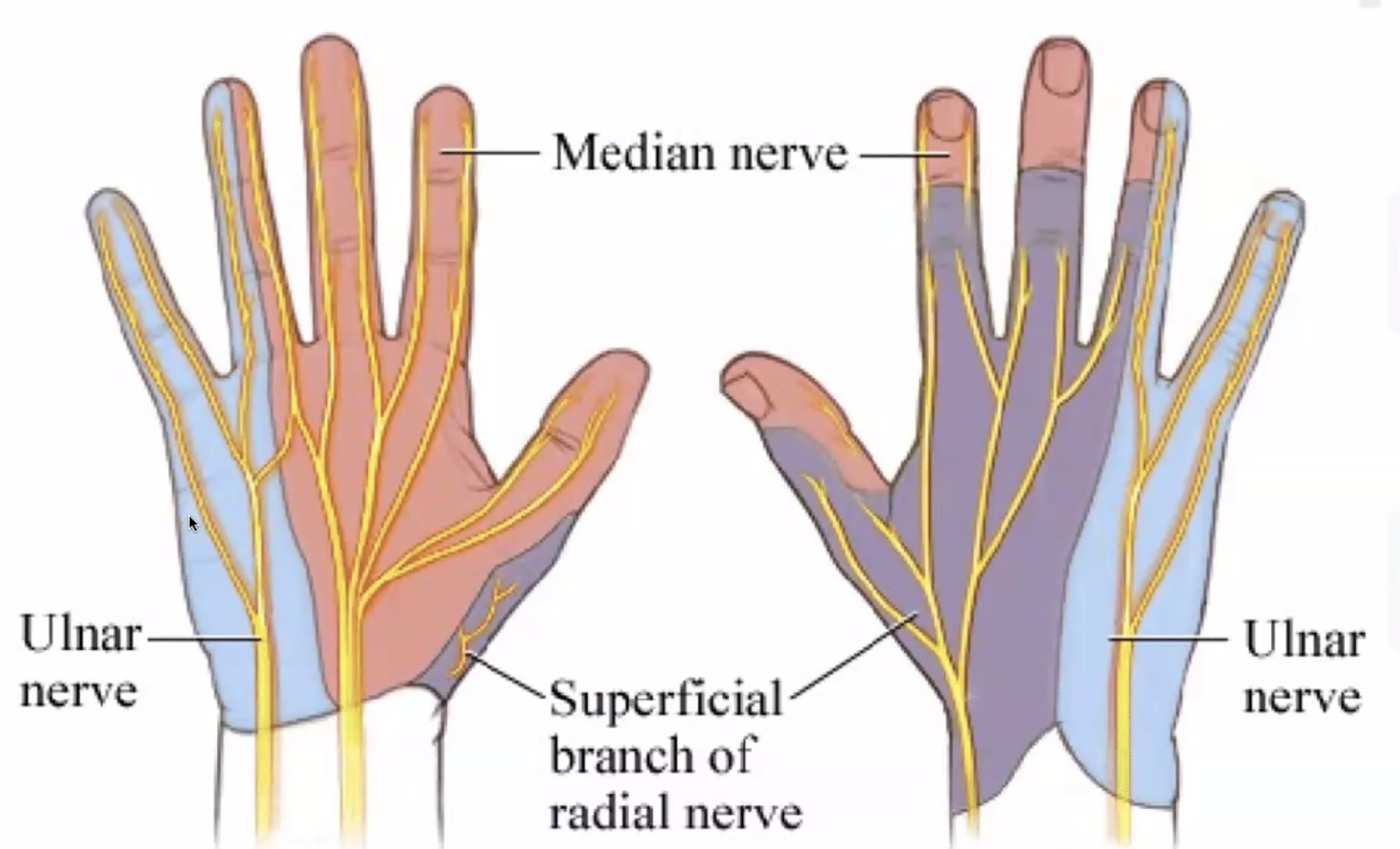
Peripheral neuropathies typically involve the sensory, motor, or autonomic nerves that branch from the spinal cord and extend throughout the limbs and trunk. These conditions frequently affect the hands and feet, where long nerve fibers are most vulnerable to damage. Common examples include carpal tunnel syndrome, where compression of the median nerve in the wrist leads to numbness and tingling in the hand, and diabetic peripheral neuropathy, which often presents as burning pain, numbness, or weakness in the feet and lower legs. Other presentations may involve post-herpetic neuralgia, sciatic nerve irritation, or thoracic outlet syndrome.
Cranial neuropathies, by contrast, affect the 12 cranial nerves, which emerge directly from the brainstem and innervate structures in the head, neck, and thoracic cavity—including the vagus nerve (cranial nerve X), which plays a crucial role in regulating autonomic functions like heart rate, digestion, and inflammation.
Neuropathies can be:
Sensory: affecting how the body feels pain, touch, or temperature.
Motor: impacting voluntary muscle control.
Autonomic: disrupting involuntary functions like breathing, heart rate, digestion, or blood pressure.
Or mixed, affecting several modalities at once.
At the neurophysiological level, neuropathy may involve:
Axonal injury: damage to the long fibers that carry electrical signals.
Demyelination: deterioration of the insulating myelin sheath, impairing signal speed and precision.
Neuroinflammation and immune-mediated processes: where local or systemic inflammation disrupts nerve function and regeneration.
Altered ion channel expression and ectopic discharge, leading to chronic pain or abnormal nerve firing patterns.
Treating Peripheral Neuropathies with Electro-Acupuncture: Afferent and Efferent Fiber Targeting
Peripheral neuropathies involve either sensory (afferent) or motor (efferent) nerves—or sometimes both. Understanding this distinction is essential to tailoring treatment with electro-acupuncture in a way that supports neuroregulation, nerve repair, and functional restoration.
Afferent (Sensory) Peripheral Nerves
Afferent fibers carry information toward the central nervous system (CNS). These nerves are responsible for transmitting sensations such as pain, temperature, vibration, and touch from the periphery (like the hands or feet) to the spinal cord and brain.
In my clinical practice, I often assess which fiber types are likely involved based on symptom quality and distribution:
C-fibers: These unmyelinated, slow-conducting fibers are involved in dull, burning, or aching pain and in sensations of warmth or heat. They’re often overactive or damaged in chronic pain syndromes, including diabetic foot neuropathy or post-injury nerve sensitivity. I use low-frequency, gentle electro-acupuncture at distal points to help desensitize these pathways and reestablish appropriate pain signaling.
A-delta fibers: Lightly myelinated and faster than C-fibers, these transmit sharp, localized pain and cold. They are typically engaged in more acute or mechanical pain. When treating conditions like carpal tunnel syndrome, where nerve compression causes tingling or sharp discomfort, I may use moderate-frequency stimulation targeting specific local channels to modulate A-delta activity and reduce hyperexcitability.
A-beta fibers: These myelinated fibers carry touch, pressure, and vibration sensations. In cases of sensory loss, I stimulate areas associated with A-beta input to help promote neuroplasticity and re-engage cortical sensory mapping.
By tailoring my frequency and needle placement to match the affected fiber type, I aim to normalize nerve function, reduce aberrant pain signals, and encourage sensory reintegration in affected regions.
Efferent (Motor) Peripheral Nerves
Efferent fibers carry signals away from the CNS to the body, particularly to muscles. Damage to these nerves can result in muscle weakness, atrophy, or poor motor control—commonly seen in conditions like foot drop, radiculopathies, or post-stroke weakness.
Electro-acupuncture allows me to engage different efferent fibers depending on the patient’s presentation:
A-alpha fibers: These are large, fast-conducting motor neurons responsible for voluntary muscle contraction. When these are affected—such as in sciatic neuropathy—I often use mid-frequency electro-stimulation on motor points to recruit muscle activation and encourage neuromuscular re-education.
A-gamma fibers: These smaller motor fibers regulate muscle spindle sensitivity, playing a role in tone and reflex regulation. In cases of spasticity or postural imbalance following nerve injury, I target deep muscular layers using fine-needle techniques and precise electro-stimulation to help reset proprioceptive control and improve functional mobility.
Targeting Cranial Neuropathies: Vagus Nerve Regulation Through Auricular Electro-Acupuncture
While peripheral neuropathies often affect the limbs, cranial neuropathies can involve key nerves emerging directly from the brainstem—including the vagus nerve (cranial nerve X), which plays a crucial role in regulating the autonomic nervous system.
The vagus nerve innervates the heart, lungs, digestive tract, and has strong influence on inflammatory tone, stress resilience, mood, and organ regulation. It also carries 80% afferent fibers, meaning it transmits vast amounts of sensory information from the body to the brain—making it a powerful pathway for neurofeedback and self-regulation.
Auricular Access: The Cymba Concha Connection
Good news! One of the few places on the body where the vagus nerve reaches the surface is the cymba concha of the external ear. This region is innervated by the auricular branch of the vagus nerve (ABVN), allowing for non-invasive stimulation of the vagal system (Verma et al., 2021).
In my clinic, I use low-frequency (25 Hz) mili current stimulation applied to acupuncture points in the cymba concha to activate vagal afferents. This method, known as auricular vagus nerve stimulation (aVNS), has been shown in studies to modulate:
Heart rate variability (HRV) (Machetanz et al., 2021)
Inflammatory cytokine levels
HPA axis function
Mood disorders such as anxiety and depression
Research demonstrates that 25 Hz mili current stimulation at the cymba concha can enhance parasympathetic tone, downregulate sympathetic overactivity, and promote a state of physiological calm, which is crucial for recovery in cases of autonomic dysregulation, functional gastrointestinal disorders, chronic fatigue, and long-COVID neuropathy (Sclocco et al., 2020).
